If you're trying to get pregnant and have questions about endometriosis, you're in the right place. Sure! Here's a natural rephrasing of that sentence:
Around 30% to 50% of women with endometriosis experience infertility, according to the American Society for Reproductive Medicine — and many only find out when they begin fertility evaluations.
This article will help you understand can endometriosis cause infertility, what it means for your fertility, and the steps you can take — from recognizing endometriosis symptoms to exploring options like in vitro fertilization or intrauterine insemination.
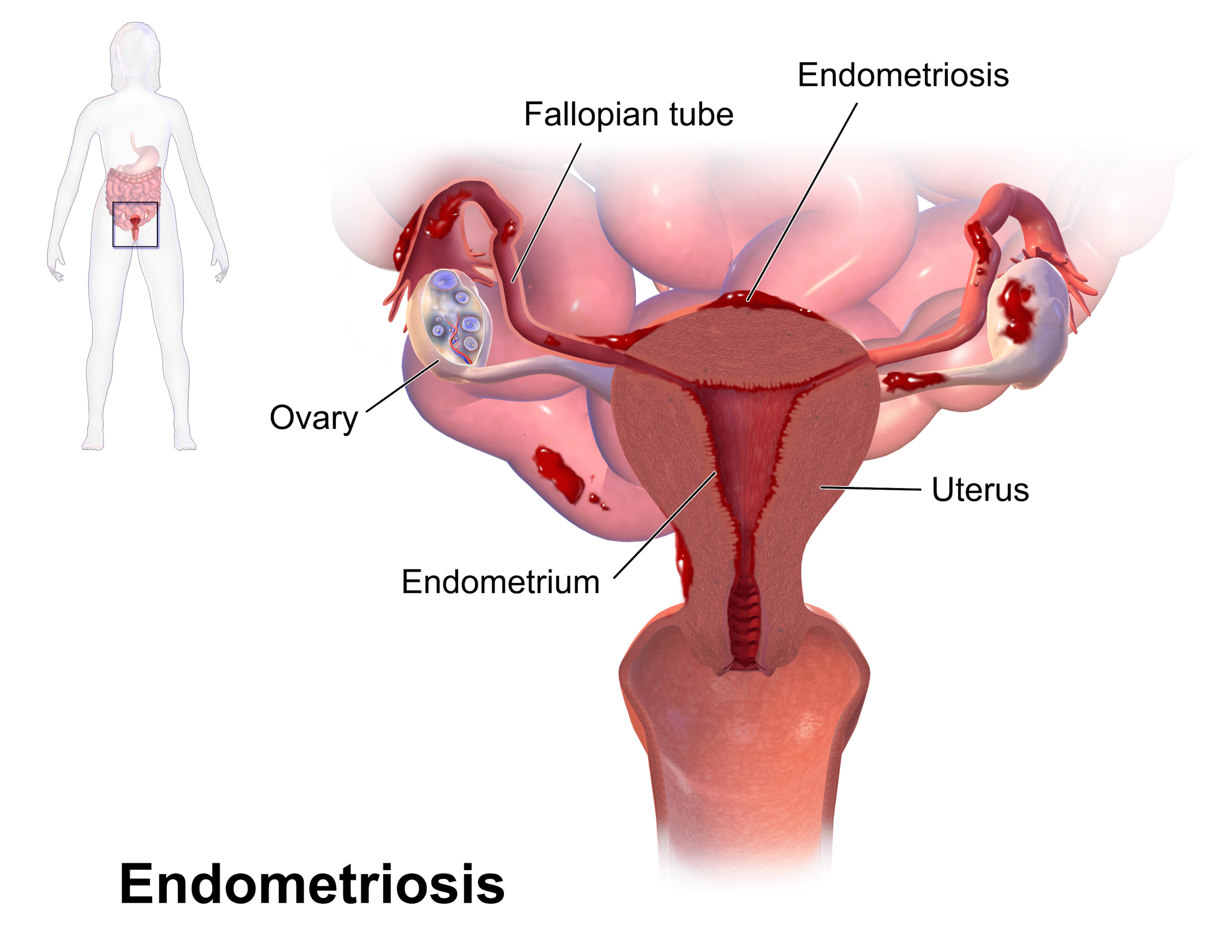
What Is Endometriosis?
If you've been told you might have endometriosis, you're probably wondering what that even means. It can be confusing — especially when symptoms vary from person to person. But knowing what’s actually happening inside your body helps you take the right next step.
Endometriosis happens when endometrial-like tissue grows outside the uterus, where it shouldn’t be. These cells behave like normal endometrial tissue, responding to your menstrual cycle, but they don’t have a way to exit the body. That’s what causes pain, inflammation, and over time, complications with fertility.
According to the World Health Organization, it affects about 10% of reproductive-age women globally — many of whom may be undiagnosed for years.
"Want expert help in understanding your symptoms before trying to conceive? Consult Dr. Anshu Agarwal for personalized guidance and support that’s grounded in real experience."
How Can Endometriosis Affect Fertility?

If you've been diagnosed with endometriosis or suspect it, one of the biggest questions on your mind might be: can this affect my ability to get pregnant? The short answer is yes — but it’s not the same for everyone.
The way it impacts fertility depends on where the tissue grows, how your body responds, and how early it’s managed.
1. Symptoms that interfere
Some people deal with intense pelvic pain, while others don’t even realize they have it. The issue is that menstrual period symptoms don’t always match the severity of the condition.
That’s why deep endometriosis or minimal and mild endometriosis can both interfere with fertility without obvious warning signs.
- Endometriosis may cause:
- Severe pain in the lower abdomen
- Ongoing chronic disease that worsens with time
- Abdominal pain mistaken for other issues like IBS
- Endometriosis associated pain that interferes with intimacy and comfort
2. Fallopian tube damage
When ectopic endometrial tissue grows near the tubes, it can cause pelvic adhesions or even block the path completely.
This can lead to tubal factor infertility and lower your chances of natural conception. Scarred tubes may not allow eggs and sperm to meet.
- Adhesions and scar tissue can:
- Obstruct tubal function
- Alter pelvic anatomy
- Increase risk of ectopic pregnancy
3. Inflammation and eggs
The condition often triggers a chronic inflammatory reaction in the pelvic cavity. That can damage eggs or reduce their quality.
“The increased volume of peritoneal fluid in endometriosis patients may impair sperm and egg function,” says the American Society for Reproductive Medicine.
- This can lead to:
- Decreased ovarian reserve
- Dysfunctional endometrial receptivity
- Formation of ovarian endometrioma
4. Hormonal disruption
Even if you ovulate regularly, ovulation suppression from hormonal imbalance can quietly impact fertility. This is more common in those with moderate endometriosis or minimal mild endometriosis.
And while oral contraceptives and birth control pills may ease pain, they’re not ideal if you're trying to conceive.
5. Associated infertility factors
Sometimes, endometriosis shows up alongside other fertility barriers. These include male factor infertility, unexplained infertility, or a history of previous ovarian surgery. All these can lower pregnancy rates, especially in infertile women.
- What to discuss with your doctor:
- Do you need diagnostic laparoscopy?
- Is surgical treatment or surgical excision an option?
- Could vitro fertilization embryo transfer improve your chances?
Understanding these connections helps you make more informed choices — and feel more in control of your journey.
What are the Common Endometriosis Symptoms you Shouldn't Ignore

Endometriosis symptoms can sneak up on you. Sometimes they’re intense, and sometimes they’re easy to brush off as “normal.”
But if any of these signs show up often, it’s worth paying attention — especially if you’re planning to get pregnant.
1. Painful periods
This is one of the most common red flags. If your menstrual blood flow feels unusually heavy or your cramps keep you in bed, that’s not something to ignore. Pain may be caused by endometriosis tissue reacting during your menstrual cycle.
- Also linked to:
- Discomfort from retrograde menstruation
- Repeated inflammation in the peritoneal endometriosis areas
- Early signs of ovarian stimulation imbalance
2. Chronic pelvic pain
This pain might feel dull or sharp, and it doesn’t always line up with your period. Some people experience it for years before getting a diagnosis.
Laparoscopic surgery is often the first way doctors spot it.
- It could indicate:
- Endometriosis lesions or deep tissue buildup
- Disruption in your normal pelvic anatomy
- Long-term chronic disease that needs attention
3. Pain during intercourse
Painful sex isn’t just physical — it affects your relationship and confidence too. In some cases, treating endometriosis through medical treatment or surgical excision can bring relief. But proper diagnosis is key.
4. Heavy menstrual bleeding
If your period often lasts longer than 7 days or soaks through products in under an hour, talk to your doctor.
This isn’t just inconvenient — it’s a symptom. It may be caused by endometrial cells growing where they shouldn’t.
5. Digestive or bladder issues
Bloating, cramping, or frequent urination? These are sometimes misdiagnosed as irritable bowel syndrome.
But when paired with period pain, they might actually signal peritoneal endometriosis or nearby endometriosis tissue growth.
6. Difficulty getting pregnant
This is how many people first discover they have endometriosis. If you've been trying for a while with no luck, consider asking your doctor about a diagnostic laparoscopy.
As noted by Fertility and Sterility, a leading journal in reproductive medicine, "unexplained infertility" is often found to be early-stage endometriosis.
- Discuss options like:
- Fertility therapy after diagnosis
- Next steps if clinical pregnancy hasn’t occurred
- Managing symptoms while you treat pain and plan ahead
Catching symptoms early can make all the difference. You're not overreacting — you're taking care of your future.
Can Endometriosis Cause Infertility in All Women?

Not all women with endometriosis struggle to get pregnant — but some do. So, can endometriosis cause infertility in all women?
The truth is, it depends on the stage, your symptoms, and how your body responds to treatment.
Mild vs. Severe Cases: Does Severity Always Affect Fertility?
It might surprise you, but mild endometriosis can sometimes cause more trouble than severe endometriosis. That’s because fertility issues aren’t always about how much tissue is present — it's about where it grows and how it interferes with your reproductive system.
For example, even minimal scarring near the fallopian tubes can cause a blockage.
- In clinical observations:
- Severe disease may cause obvious damage, but many women with minimal or mild endometriosis still experience infertility
- Some women with advanced stages still conceive naturally
- According to Fertility and Sterility, outcomes vary more by location than by stage
A randomized controlled trial published in the Cochrane Database noted that surgical removal of visible implants in minimal to mild stages can improve chances of pregnancy. Still, it’s not a guaranteed fix.
Why Endometriosis-Related Infertility Is Often Misunderstood

One major issue is that the symptoms don’t always match what’s happening inside. Some women may have no pain or signs at all, yet still face fertility struggles.
These are often labeled as infertile patients with “unexplained infertility” until further tests reveal endometriosis tissue or inflammation.
- The condition is often misunderstood because:
- It overlaps with other issues like hormonal disorders or even male factor infertility
- It isn’t always visible without laparoscopic surgery or specialized scans
- It's sometimes dismissed unless there is severe pain or heavy bleeding
Early diagnosis matters, especially for women hoping to conceive soon. According to the American Society for Reproductive Medicine, many fertility-focused clinics now advocate for proactive testing when endometriosis is suspected — even in the absence of obvious symptoms.
There’s ongoing research into the role of stem cells and how they influence treatment of endometriosis in future therapies.
But for now, the key is awareness, timely care, and a personalized plan that aligns with your reproductive goals.
How Is Endometriosis Diagnosed Before Conception?

If you're trying to conceive and suspect endometriosis, the first step is getting a proper diagnosis. But since symptoms don’t always match the severity, it’s not always easy to spot. That’s why many women only discover it during fertility checkups.
Doctors usually start by asking about your menstrual cycle, pain patterns, and any history of pelvic pain or painful sex. But to confirm endometriosis, imaging and sometimes surgery is needed.
The gold standard for diagnosis is laparoscopic surgery — a minimally invasive procedure that lets doctors see and remove endometriosis tissue.
Common diagnostic steps include:
- Pelvic ultrasound
- Can detect larger cysts like ovarian endometrioma
- But may miss smaller or hidden lesions
- Diagnostic laparoscopy
- Visualizes and removes ectopic endometrial tissue
- Helps confirm the stage and plan surgical treatment
- Blood tests and symptom mapping
- Often used to support, but not confirm, diagnosis
If you're planning pregnancy soon, don’t wait too long to investigate persistent symptoms.
Early diagnosis improves your chances — not just of managing pain, but also of making informed decisions about fertility.
What Should You Do Before Trying to Conceive?

Thinking about pregnancy while dealing with endometriosis can feel overwhelming. But you don’t have to wait until things get difficult to act.
Being proactive can save you time, stress, and heartache later.
When to Consider Seeing a Fertility Specialist
Not sure if you should see a specialist yet? Here’s a quick way to decide: if you've been trying to conceive for 6 months or more (and you're over 35), it's time to check in.
If you're under 35 and it’s been a year, go ahead and schedule that appointment.
- A fertility specialist can:
- Evaluate your full reproductive history
- Suggest personalized tests or imaging
- Guide you through possible options early on
Preconception Steps for Women with Symptoms

Even if you haven’t started trying yet, there’s value in preparing your body ahead of time. Small changes and awareness can make a big difference later.
Start by listening to your body — especially if you've had painful cycles or digestive issues.
- Smart steps to take:
- Track your cycles consistently for patterns
- Keep a symptom journal to discuss with your doctor
- Get basic hormone tests and discuss supplements if needed
- Consider low-impact movement and an anti-inflammatory diet
Why Early Planning Helps with Endometriosis and Fertility
When it comes to endometriosis, waiting and hoping things will resolve on their own rarely works. The longer the tissue grows without a plan in place, the more it can complicate fertility. Early planning gives you more time, more options, and often better outcomes.
- Planning helps you:
- Understand your fertility timeline
- Avoid rushed decisions down the road
- Feel more confident and supported with a team in place
You deserve clarity before the pressure builds. Taking small steps now can help you avoid big surprises later — and give you a better shot at the future you’re hoping for.
"Planning to start your fertility journey? Schedule a consultation with Dr. Anshu Agarwal to discuss your goals and get a care plan designed just for you."
What Are the Treatment Options That Work?

If you're thinking about pregnancy and managing endometriosis, knowing your treatment options can give you a real sense of direction.
The good news? There isn’t just one right path — it all depends on your symptoms, goals, and how your body responds.
Hormonal Treatments and Birth Control Pills: When Are They Helpful?
If you're not trying to get pregnant right now, hormonal therapy is often the first recommendation.
Birth control pills, patches, or hormonal IUDs can reduce pain by suppressing ovulation and slowing the growth of tissue.
They’re useful for symptom relief — but not if you're trying to conceive.
- When they help:
- Reducing monthly pain and cramping
- Preventing progression of active disease
- Offering control while you plan for future fertility
- When to skip:
- If you're ready to start trying soon
- If you're experiencing side effects or breakthrough pain
- If hormone suppression doesn't reduce your symptoms
Is Surgery Necessary for Endometriosis-Associated Infertility?

Surgery isn’t always the first step, but it can be effective — especially for women with moderate symptoms and structural complications.
Minimally invasive procedures can remove or destroy tissue, improve anatomy, and in some cases, improve chances of conception. However, not everyone benefits the same way.
- Consider surgery if:
- You’ve tried medications and nothing has worked
- Imaging shows tissue near reproductive organs
- You have visible cysts, adhesions, or organ distortion
- Things to keep in mind:
- Surgery has risks and recovery time
- Fertility doesn’t always improve afterward
- Some women may need more than one procedure over time
Intrauterine Insemination vs. In Vitro Fertilization — What Works Better?
Once you’re ready to try, assisted reproductive techniques like IUI and IVF may come into play. Intrauterine insemination (IUI) is a less invasive option, placing sperm directly into the uterus during ovulation. It’s often used in mild cases or when timing is the biggest hurdle.
In vitro fertilization (IVF) is more complex but also more effective — especially for moderate to severe cases. It bypasses many of the common barriers caused by endometriosis, including tubal issues and egg-sperm interaction.
- IUI may be a good fit if:
- Your tubes are open and healthy
- You have minimal symptoms
- You’re trying a step-by-step approach
- IVF might be better if:
- Other treatments haven’t worked
- There’s damage to the reproductive anatomy
- Time is a factor or egg quality is a concern
Choosing a treatment path isn’t about rushing — it’s about what’s right for you. Talk openly with your doctor, weigh your options, and trust that taking action is already a powerful step forward.
Dr. Anshu Agarwal’s Insights on Endometriosis and Fertility

Dr. Anshu Agarwal is a leading Obstetrician and Gynecologist based in Ranchi, known for her expertise in managing endometriosis and infertility.
With over 18 years of experience and a strong background in laparoscopic procedures and high-risk pregnancy care, she has helped thousands of women conceive naturally — often without needing IVF. Her approach is practical, personalized, and deeply empathetic.
Unique Insights from Dr. Anshu Agarwal:
- Endometriosis doesn’t always need aggressive treatment.
In many cases, managing pain and inflammation conservatively can help women plan pregnancy more calmly, without jumping straight into surgery or IVF. - Delayed diagnosis is still one of the biggest barriers.
Many patients normalize symptoms for years. Dr. Agarwal encourages early consultations — even if conception isn’t an immediate goal — to protect long-term fertility. - Emotional health plays a key role.
Anxiety around conception often flares up when paired with chronic pain. Dr. Agarwal emphasizes counseling and support as part of fertility care. - Not all surgeries are equal.
She stresses the importance of targeted laparoscopic excision rather than unnecessary extensive procedures that can damage ovarian function. - Natural conception is possible post minimal treatment.
For many women with early-stage endometriosis, timed intercourse after basic pain management and tracking ovulation has led to successful pregnancies under her care.
"Ready to take the first step with a doctor who truly understands endometriosis and infertility? Visit Dr. Anshu Agarwal’s website to connect and learn more."
FAQs

1. Can you still be fertile if you have endometriosis?
Yes, absolutely. Many women with endometriosis go on to have healthy pregnancies — either naturally or with the help of fertility treatments. Just because you have the condition doesn’t mean you’re infertile.
Fertility depends on several factors: how advanced the endometriosis is, where the tissue is growing, and how your body responds to treatment. Even women with mild symptoms sometimes struggle to conceive, while others with advanced stages may have no issues at all.
2. Can infertility caused by endometriosis be cured?
“Cured” isn’t always the right word, but it can be managed — and pregnancy is definitely possible. Treatments like surgery, IVF, or hormone therapy can improve fertility outcomes in many cases.
However, success rates vary. Some women respond well to laparoscopic procedures, while others may need assisted reproductive technologies to conceive. It’s all about finding what works for your body.
3. What is the fertility index for endometriosis?
The Endometriosis Fertility Index (EFI) is a clinical scoring system doctors use to predict your chances of getting pregnant after surgical treatment. It considers your age, ovarian health, fallopian tube condition, and severity of endometriosis.
The EFI helps guide decisions — like whether to try naturally, go for IUI, or consider IVF. A higher score means a better chance of natural conception, while a lower score may point toward assisted options.
4. Is endometriosis a high-risk pregnancy?
It can be — but not always. Endometriosis may increase the risk of complications like preterm birth or placental issues, especially in moderate to severe cases.
That said, many women with endometriosis have smooth, healthy pregnancies with the right prenatal care.
Close monitoring, early screenings, and a supportive OB-GYN team can make a big difference.
Conclusion
If you’ve been wondering whether endometriosis could affect your chances of getting pregnant, you’re not alone — and you’re not without options. Understanding your symptoms, getting a proper diagnosis, and planning ahead can make a real difference.
Whether it’s tracking your cycle, speaking to a fertility specialist, or exploring treatments like IVF, every step you take matters. The journey might feel uncertain at times, but it doesn’t have to be confusing.
Stay curious, stay proactive, and most importantly — know that support is out there. You deserve answers, clarity, and a path that’s right for you.
"Don’t leave your questions unanswered. Reach out to Dr. Anshu Agarwal and take control of your fertility journey with confidence and care."


.jpg)

.jpg)


